A new Xenopus model for Urofacial Syndrome
Urofacial syndrome (UFS) is an autosomal recessive congenital disorder characterized by two symptoms in different anatomical systems- the smooth muscles of the bladder, and musculature of the face. The main diagnostic features are incomplete bladder emptying during urination, and an abnormal facial expression upon smiling. A child’s a downward or inverted smile allows early detection of the disorder, which can have severe, even fatal, consequences due to renal failure if left untreated. Mutations in the human HPSE2 gene were recently identified as the cause for UFS (Daly et al, 2010. Am. J. Hum. Genet., 11, 963-969; and Pang et al 2010. Am. J. Hum. Genet., 11, 957-962.)
This latest work by Neil Roberts et al. identifies and knocks down the Xenopus orthologue of human HPSE2: it is published in the April 2014 edition of Human Molecular Genetics. This collaboration between researchers from Pediatrics and Child Health, Genomic Medicine and Developmental Biology groups at the University of Manchester, establishes for the first time, an in vivo vertebrate model for the UFS, and importantly, it is the first study to shed light on the mechanisms underpinning the clinical features of UFS.
Morpholino knockdown of the hpse2 gene in Xenopus generated tadpoles with the combination of characteristics that largely explain the human UFS condition. The observed abnormal motor neurons emanating from the trunk neural tube were associated with skeletal muscle paralysis, motility issues and a lack of escape response. Biochemical analyses demonstrated that loss of hpse2 led to upregulation of FGF2/pERK signalling and to alterations in levels of transcripts encoding neural and muscle associated molecules. Thus the authors demonstrated a requirement for normal hpse2 expression for correct peripheral motor neuron functional development in the trunk region of Xenopus tadpoles, and they further proposed that hpse2 plays a similar role in the development of peripheral motor nerves of the human face including the facial nerves, and viscera. This would explain the abnormal smile and muscular weakness observed in individuals with UFS. With regard to the bladder dysfunction, Roberts et al. argue that the two sets of motor neurons involved in correct bladder function may also be effected by hpse2 mutation.
“Thus, a key role of heparanase 2 is to buffer growth factor signalling in motor neuron development. These results shed light on the pathogenic mechanisms underpinning the clinical features of UFS and support the contention that congenital peripheral neuropathy is a key feature of this disorder.”
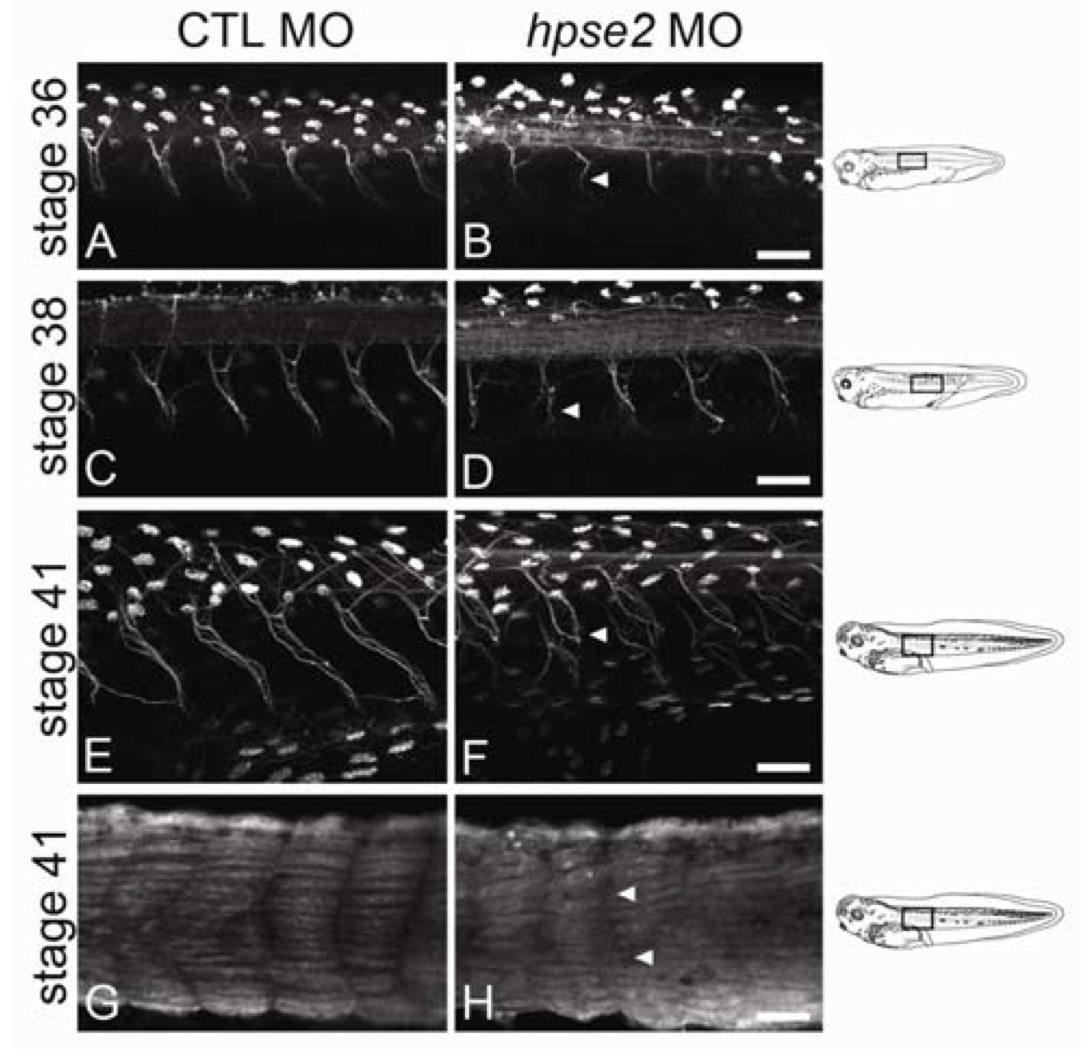
Figure 5 from Roberts et al.: The motor nerves which emanated from the neural tube in MO knockdown Xenopus occurred at regular intervals, but the average length of these nerves was shorter (although not statistically significant), their path was more meandering, and axons in these nerves were less compactly bundled.
© The Author 2014. Published by
Summary by CJZ and VGP, Xenbase scientific curators.
